Now accounting for approximately 20% of newly diagnosed breast cancer1, this early form of breast cancer pertains to the abnormal cells within the milk ducts. It has not spread outside of the milk ducts and therefore is considered non-invasive. This is considered a Stage 0 cancer. You may not feel anything, like a lump, but it can be detected on a mammogram as suspicious, abnormal branching or linear calcifications. DCIS is diagnosed by doing a biopsy of the tissue. Once diagnosed a patient is scheduled to see a breast cancer surgeon, a plastic surgeon, a radiation oncologist and a medical oncologist, and many times the patients able to see each doctor all on the same day.2 But if DCIS is considered a stage 0 cancer, is it necessary to consult with all these doctors? The problem lies here: according to Mark Mead MSc, integrative oncology research consultant, DCIS is considered “non-obligate”. This means that it may or may not turn into cancer and therefore calling it “cancer” is considered a misnomer.
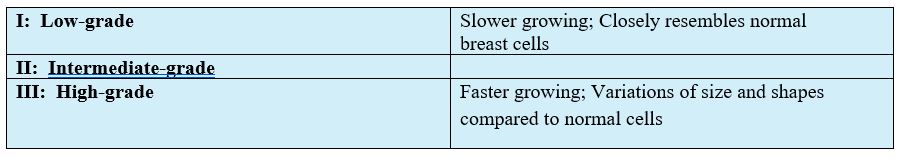
3 Grades of DCIS
Treatment
Is surgery necessary? Mead’s stats show that 98% of DCIS is treated surgically by either a mastectomy, where they remove the entire breast, or by a lumpectomy, where they remove just the area that is abnormal. Literature shows that the risk of cancer coming back into their breast in that area is about 40 percent in the next 20 years when surgery is performed.2
Currently, there are more clinical trials going on to assess whether patients with low-grade DCIS can be safely managed by an active surveillance approach, with avoidance of unnecessary treatments.3One 30 year study concluded that women with low-grade DCIS showed that only 40% developed invasive breast cancer in the absence of any treatment other than biopsy, almost a third of which were diagnosed more than 2 decades later.4 Would low-grade DCIS ever form a health hazard if left alone? What percentage of DCIS actually turns into cancer without doing surgery? Hopefully, the $6 billion raised every year for breast cancer is going to some of this research…
By electing out of surgery you avoid exposing dormant cells, in the case of DCIS, to oxygen which can lead to DNA damage. Excess DNA damage by oxidation is linked to certain diseases and cancers. DNA damage occurs every day; it is a natural part of aging. However, this damage doesn’t repair 100%. When there are errors that occur with repair or replication, this can cause DNA mutation. The mutation of these cells is what can contribute to and possibly progress to cancer.
After surgery, radiation and/or chemotherapy is recommended depending on the grade of the DCIS. The follow up recommendations for women diagnosed with DCIS are usually 5 years of endocrine therapy, if tested hormone receptor-positive, along with annual mammograms. However, if a patient diagnosed with DCIS is known to already have abnormal cells, why would you expose those abnormal cells to radiation from a mammogram?
In 1995 the British medical journal The Lancet reported that, “since mammographic screening was introduced in 1983, the incidence of ductal carcinoma in situ (DCIS), which represents 12% of all breast cancer cases, has increased by 328%, and 200% of this increase is due to the use of mammography. This increase is for all women: Since the inception of widespread mammographic screening, the increase for women under the age of 40 has gone up over 3000%.5”
Instead of mammography screening for these women that are now placed in a higher risk category, Thermography screening would be useful. Thermography is a screening tool that can detect changes in the breast tissue by providing accurate and reproducible images of the breast without the use of radiation and compression. The screening device is approved by the FDA and is a much safer way to monitor these women with already abnormal cells. There is a huge role that thermography can play in detecting the progression of DCIS into IBC (invasive breast cancer). A woman can be monitored as often as four times a year and there would be no exposures to any sort of radiation or compression. This type of screening is especially useful for women who have dense breasts. Mead’s literature reviews and research brings up the discussion on the sensitivity of mammography in women with DCIS and high breast density. At the 2019 American Academy of Thermology session, Mead presented on DCIS and the future of thermography. Mead states “Mammography will never be 100% due to breast density, but there is a role for thermography here with sensitivity being 97-100%.”
As mentioned before, an active surveillance program would be of interest to women with lower risk factors. For instance, The US Preventative Services Task Force (USPSTF) currently does not recommend routine screening for women in their 40s, but rather recommends a discussion of the risks and benefits.6 In this age group, the chance of absolute benefit is lowest and the chance of false-positives highest.6The available data suggest that in making screening recommendations based on and individual’s risk profile, overdiagnosis can be minimized and the potential benefit will be maximized.
Within a patient’s risk profile, metabolic trends seen in blood work can also be useful because it is non-invasive and also reproducible. Testing a comprehensive blood test along with cancer markers such as CA27.29, CA15-3, and LASA as well as heavy metal testing, can determine a patient’s health status at a metabolic level. Deficiencies, toxicities, immune function, hormone balance, and inflammation can all be seen in the blood. Placing patients on personalized supplement protocols and dietary guidelines based on their comprehensive testing results monitoring changes seen in the blood will benefit the patient’s overall health. Preventing DCIS turning into invasive cancer, or even just slowing it down, is the goal when speaking of an “active surveillance program”.
Blood testing and heavy metal testing can be done at any age. It is never too late to start. You may even be surprised at findings that can be detected on comprehensive blood panels that go above and beyond what your primary doctor is testing. Wouldn’t it be useful to note that your diabetic marker is going up before you become diabetic? Instead of waiting until a diagnosis is made, be preventive, be proactive, and be educated about your health. Set up your appointment today to discuss benefits of blood testing and heavy metal testing to see where you need to make changes in your lifestyle and start your “active surveillance program”!
References
- Armed Forces Health Surveillance Center. Incident diagnoses of breast cancer, active component service women, U.S. Armed Forces, 2000- 2012. MSMR 2013; 20:25–27
- Koty, Patrick P. “Breast Cancer Prevention by Inducing Apoptosis in DCIS Using Breast Ductal Lavage.” 2005, doi:10.21236/ada443722.
- C.J. Wright and C.B. Mueller, «Screening Mammography and Public Health Policy,» The Lancet, July 1995.
- Elshof LE, Tryfonidis K, Slaets L, et al. Feasibility of a prospective, randomized, open-label international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ—the LORD study. Eur J Cancer 2015; 51: 1497–510. 25 Gotzsche PC,
- Sanders ME, Schuyler PA, Dupont WD, Page DL. The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer 2005;103:2481–2484.
- Mandelblatt JS, Cronin KA, Bailey S, et al. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med 2009;151:738–747.

